Thierry Naas: The fight against antibiotic resistance
Thierry Naas is a lecturer at Université Paris-Saclay, and a hospital practitioner at Bicêtre Hospital. Based in the Immunology of Viral, Auto-immune, Hematological and Bacterial Diseases laboratory (IMVA-HB - Univ. Paris-Saclay, Inserm, CEA), he works to curb the spread of antibiotic resistance in bacteria within the human digestive tract. This resistance compromises the treatment of bacterial infections in patients, including hospitalised patients, who are often the most vulnerable.
We humans have a complicated relationship with the bacteria in our intestines, the most famous of which is: Escherichia coli (E. coli). "E. coli is simultaneously our best friend and our worst enemy. We live in symbiosis with it, but only when we are healthy. The slightest weakening of our immune system allows E. coli to infiltrate into places where it is not welcome, thereby causing opportunistic infection," explains Thierry Naas, director of the Emerging Resistance to Antibiotics (RESIST) team within the Immunology of Viral, Auto-Immune, Hematological and Bacterial Diseases laboratory (IMVA-HB - Univ. Paris-Saclay, Inserm, CEA).
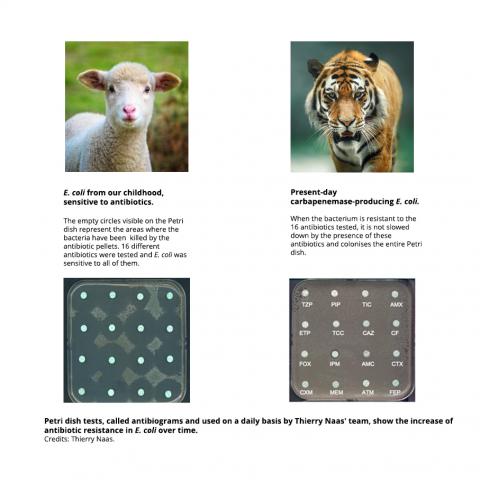
Taking antibiotics generally kills these out-of-control bacteria. But antibiotics sometimes lose their efficacy. As a result of random mutations in its DNA or if it takes over genetic material from another bacterium, a bacterium can become resistant to an antibiotic. This antibiotic resistance can then be transmitted from one bacterium to another, owing to their ability to exchange fragments of DNA through mobile genetic elements. "How do these mobile elements move? Which factors increase or decrease the frequency of transmission and integration in the genome? What are the consequences for bacteria?" questions Thierry Naas, whose research is centred on the mobility of DNA.
Understanding antibiotic resistance through mobile DNA
Ever since he started his higher education studies, Thierry Naas has been fascinated by health and infectiology. After two years at Université Louis Pasteur (Strasbourg), he studied at the École supérieure de biotechnologie de Strasbourg (ESBS). "I then had the chance to do my end-of-study internship in the HIV department of the pharmaceutical company Roche, in Basel (Switzerland)." There, the young researcher discovered the process of developing new drugs to combat the AIDS virus, working on viral proteins and their inhibitors.
With his engineering degree and his DEA (Diploma of Advanced Studies, the equivalent of a 2nd year of Master's degree in research today) under his belt, he decided to continue his career in university research. "I was drawn to the intellectual freedom offered by the academic world," Naas recalls. He completed his thesis on mobile elements, called 'insertion sequences', at the University of Basel, in the laboratory of Werner Arber, winner of the Nobel Prize in Medicine in 1978 for the discovery of restriction enzymes. "It was an incredible opportunity. I learned a lot about bacterial genetics from working with him and the huge potential for adaptation and mutation in E. coli." At the same time, he worked with Patrice Nordmann on the characterisation of the first resistance genes to carbapenem antibiotics.
The researcher subsequently completed a post-doctoral programme at the University of Pennsylvania (USA) in the laboratory of Haig Kazazian and worked on other mobile elements, this time present in mammals: the LINES (Long interspersed nuclear elements) retrotransposons. In 1997, he was hired as a lecturer/hospital practitioner (MCU-PH in French) within the Faculty of Medicine at Université Paris-Sud (now Université Paris-Saclay) to continue his work on emerging mechanisms of antibiotic resistance.
Resistant bacteria
Thierry Naas' cross-hairs are on the bacteria present in the digestive tract of humans, also called enterobacteria. Harmless in everyday life, they can be fatal in hospitalised individuals with weakened immune systems, such as transplant recipients, individuals undergoing chemotherapy or individuals in intensive care. In these cases, antibiotics are their only remedy against bacterial infection.
At Bicêtre Hospital, Thierry Naas co-directs the National Reference Centre (NRC) for Antibiotic Resistance to Carbapenemases, where he works hard to preserve the efficacy of antibiotics such as carbapenems, used as a last resort to treat severe Gram-negative infections. These act against multi-drug resistant bacteria, on which conventional antibiotics no longer have any effect. Unfortunately, the emergence of new resistance compromises these super-antibiotics. "Some bacteria can now produce enzymes, called carbapenemases, that degrade carbapenem antibiotics. Apart from the fact that these bacteria are resistant to treatment, they also spread very quickly." If no steps are taken to control their spread in the hospital environment, they cause a hospital epidemic within a few days.
The hospital strikes back: search and isolate
Although there has been a recent increase, few enterobacteria in France possess these enzymes for the time being. But the prevalence is much higher in other countries. "A person who has been repatriated or who has recently travelled abroad can introduce carbapenem-resistant bacteria into a French hospital. It was therefore necessary to develop rapid and effective tests for hospitalised individuals returning from a high-risk country." In collaboration with the CEA, Thierry Naas' team developed immuno-chromatographic tests, including the NG-Test CARBA 5 sold by the company NG Biotech, which has become the benchmark test for detecting carbapenemases in over 70 countries. In French hospitals, as soon as resistance to carbapenems is identified, the French National Authority for Health (HAS) recommends immediate isolation of the infected or colonised individual, putting in place dedicated staff, and even housing all these patients together in a dedicated care unit, in order to avoid any spread within the hospital. "Thanks to the efforts made, French hospitals have lived up to the image of a village of indomitable Gauls. Less than 1% of enterobacteria strains are resistant to carbapenem antibiotics, compared to 30-70% in some of our European neighbours."
A multi-faceted multi-tasker
Thierry Naas is one of the few scientists to have held the position of MCU-PH, and he divides his time between working in the hospital, teaching at Université Paris-Saclay and academic research in his laboratory. Within the IMVA-HB unit, he heads the RESIST team, which is housed in the new premises of the Faculty of Medicine Paris-Saclay, at Kremlin-Bicêtre. "Every aspect of my job demands a lot of time and commitment. But this multi-disciplinary aspect is priceless, because the subjects we research in the laboratory come from clinical observations made on our own patients." An organisation at the basis of a virtuous circle: as it is based within the hospital, the team develops clinical studies and then improves hospital care. "For example, thanks to a new immuno-chromatographic test, we will hopefully soon be able to detect resistance in as little as 15 minutes directly from clinical samples, compared to two days currently."
The future of antibiotics
The RESIST team also conducts fundamental research into the relationship between the structure and activity of bacterial enzymes which are capable of inactivating antibiotics, and epidemiological analyses to understand the spread of carbapenem resistance at the regional, French or even global level. Thanks to a collaboration with the Institute of the Chemistry of Natural Substances (ICSN - Univ. Paris-Saclay, CNRS), the Institute of Molecular Chemistry and Materials of Orsay (ICMMO – Univ. Paris-Saclay, CNRS) and the CEA, the team is developing enzyme inhibitors that destabilise the bacterial onslaught. "We are not yet witnessing the end of antibiotics, but the situation is still alarming. We are counting on public research to innovate and find new ways to tackle multi-drug resistant bacteria, and counting on the medical world to apply the means to fight these bacteria and apply best practice as regards antibiotic use, in order to preserve these drugs as long as possible".