Making mental illness visible – a challenge for MRI
(This article was originally published in L'Édition No.17)
To aid research into mental health, scientists at Université Paris-Saclay are investigating how the human brain functions using more efficient and specialised imaging equipment augmented by artificial intelligence.
The principle of MRI scanning, for which researchers Paul Lauterbur (from America) and Peter Mansfield (from the UK) were awarded the Nobel Prize for Medicine in 2003, is based on the phenomenon of magnetic resonance associated with the magnetic properties of certain atoms – and the hydrogen nucleus in particular. These nuclei point in the same direction when placed in a magnetic field generated by powerful superconducting magnets. Radio frequency pulses are then used to disturb them, much in the same way as a flick of a wrist would destabilise a spinning top without making it fall. The nuclei accumulate energy, which is released when the stimulation is stopped and they return to their original alignment. This signal is picked up by receiving antennas and interpreted to produce two or three dimensional images.
Hydrogen is present in large quantities in the human body and can be largely found in water molecules. It is the H in H2O. The more hydrogen a tissue contains, the more effective the MRI scans. As the brain comprises 80% water, this technology is most frequently used to study its anatomy and how it functions. Compared to other non-invasive imaging techniques, MRI scans better identify tissues with a differing composition. They also have the advantage of not emitting ionising radiation, unlike X-rays or CT scans. MRI scanning is complex and still expensive. However, it is now benefiting from an opportune combination of recently successfully concluded techniques which will be able to help with mental health research.
Iseult – a 132-tonne newborn
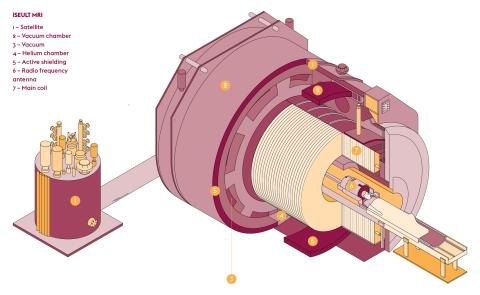
The last quarter of 2021 has culminated in a major event, namely the release of the first images from the Franco-German Iseult MRI project. This is the world’s most powerful MRI scanner for human imaging, which started operation in 2017 at the NeuroSpin centre (Univ. Paris-Saclay, CEA) at CEA Saclay. The instrument is the result of an international cooperation between academic and industrial partners which began in 2006 (CEA, the University of Freiburg, Bruker Biospin, Alstom now part of General Electric, Guerbet and Siemens Healthineers). Images have been released of a pumpkin, chosen for its water content and texture similar to the human brain, with a resolution of 400 microns in all three dimensions. Although even more powerful MRI scanners are already in use for research into materials science, preclinical research on small animals and in industry, most hospital equipment operates at a magnetic field of between 1.5 and 3 Teslas (T). The Iseult MRI scanner, with its 11.7 T, aims to increase the resolution of images currently produced in medical brain research by a factor of ten to one tenth of a millimetre and to reduce the time required to create the image. With all this taken into consideration, the quality of the images obtained from the test on the pumpkin was a good sign.
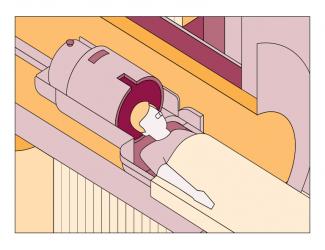
The production of such a magnetic field (equivalent to 230,000 times the Earth’s magnetic field) requires machinery of immense dimensions. It weighs 132 tonnes, is 5 metres in length and 5 metres in diameter and has a central tunnel measuring 90 centimetres in diameter. The heart of this device is a superconducting coil, formed by 182 kilometres of cables wound in rings and cooled to -271.35°C by “superfluid” helium.
This extraordinary MRI scanner will undergo several improvements over the next few months to reach a resolution of 100 to 200 microns, before it is put into service and the first images are taken from a human being. The European Aroma project, which began in 2012, aims to develop a methodology which will result in the optimal operation of the scanner. Lastly, authorisation from health authorities will give the green light for use in research into cognitive science and brain disorders.
kT-points used for fuzzy MRI images
However, increasing the magnetic field can create new problems, such as visual artefacts which degrade the image quality. These adverse effects are a direct result of the increased frequency of the radio-frequency excitation pulses used in high-field MRI scanners. At 3 T, their useful frequency is 125 MHz. It is 300 MHz at 7 T and reaches 500 MHz at 11.7 T. The wavelength is inversely proportional to the frequency, i.e. one decreases as the other increases. When the wavelength used becomes smaller than the object observed, artefacts start to appear. Alexis Amadon and his team at the Building large instruments for neuroimaging: from population imaging to ultrahigh magnetic fields unit (BAOBAB – Univ. Paris-Saclay, CEA, CNRS) at NeuroSpin have wrestled with this problem. “In the case of a 7 T MRI scanner, the wavelength of the pulses used (about 12 cm) is smaller than the average size of the brain. Areas of shade can be seen on the images as well as a loss of contrast.” This loss of contrast is particularly vexing when studying the human brain as it is divided into white and grey matter.
Alexis Amadon became interested in developing technical solutions to overcome these difficulties. His research resulted in a patent application in 2010 which was filed together with Martjin Cloos, who was a PhD student at the time. The pair had developed a method which ensured a uniform excitation pulse. “To eliminate artefacts, we interspersed very short pulses with the excitation wave trains,” explains Alexis Amadon. Called “kT-points”, this transmission method significantly improved the quality of high-field MRI images. This was so much the case that it attracted the attention of Siemens, a leading player in the field of MRI scanners, who intends to implement it on its machines. In the meantime, several clinical studies have already benefited from this technology, including one at 7 T on patients with multiple sclerosis. For the BAOBAB team, the next step is to dispense with the calibration phase prior to the clinical imaging sequences, which would bring undeniable benefits to both patients and practitioners. The development of technologies to support the increased magnetic fields of MRI scanners is set to continue.
Mood disorders, the mystery treatment
Josselin Houenou, who is director of the psychiatry team at the Clinical and Translational Neuroimaging Research Unit (UNIACT – Univ. Paris-Saclay, CEA) at NeuroSpin, and Fawzi Boumezbeur, who is from the BAOBAB team, are both looking into the other possibilities offered by high-field MRI scanners. More powerful MRI scanners permit the detection of elements other than hydrogen, such as carbon, sodium, phosphorus and lithium. As Josselin Houenou points out, “The mechanism of action of lithium is largely unknown, even though it has been the standard treatment for the mental condition known as bipolar disorder for over 70 years.” This chronic, severe psychiatric illness affects 1% of adults. Josselin Houenou’s and Fawzi Boumezbeur’s work have revealed an accumulation of lithium in the left hippocampus of bipolar patients under treatment for the first time. These results were obtained thanks to a specific piece of equipment. This was a 7 T MRI scanner suitable for this type of imaging. “There are very few laboratories in the world which have this type of dedicated equipment. We’re the first in France to make these images at 7 T,” explains Fawzi Boumezbeur.
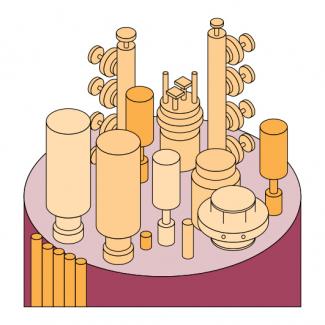
Being able to pinpoint this element, which is so much less plentiful in the human body, required the development of specialist equipment. At 7 T, the resonance frequency of lithium is 120 MHz, while that of hydrogen is 300 MHz. The same antenna just cannot be used for these two elements. “The same antenna operating with the same efficiency and sensitivity profile over such a range of frequencies would result in a loss of performance and a higher sensitivity to noise,” explains Fawzi Boumezbeur. For the moment, the mechanism of action of lithium remains unclear. However, as Fawzi Boumezbeur points out, “We now have a tool which allows us to detect the presence of lithium at an anatomical level.” This will help investigate the cellular, metabolic and genetic modalities of the currently elusive functioning of this treatment.
Psychotic disorders – connections are made
Another possibility in the field of mental health offered by high-field MRI scanners concerns the emergence of psychotic symptoms. A recent study led by Josselin Houenou showed for the first time “A link between abnormalities in the connections between different areas of the cerebral cortex, access to consciousness and the appearance of symptoms, such as delusions or hallucinations.” This result, obtained in particular thanks to experiments using diffusion MRI tractography carried out by a team from the BAOBAB unit, highlighted the bundles of neurons linking different areas of the brain. This recent technique is based on the intracellular movements of water molecules. In a spherical space, these movements occur in all directions equally. However, in nerve fibres the movement is restricted to one direction. By observing the orientation of the movement of intracellular water molecules, scientists can trace the pathways of the connections between brain structures.
“In bipolar and schizophrenic patients, psychotic symptoms are associated with poorer long-distance connectivity, particularly in the network of conscious access,” explains Josselin Houenou. Members of his team have measured the threshold of conscious perception in healthy control participants, people with a bipolar disorder with or without psychotic symptoms and people with a schizophrenic disorder. To do this, they examined the time between the presentation of a stimulus and its conscious perception. According to Josselin Houenou, “This threshold is higher in patients showing psychotic symptoms. Auditory verbal hallucinations then occur due to a lack of communication between sensory areas and the integration areas.”
Artificial neurons for human cognition
The increasing volume and complexity of diffusion MRI data requires new ways of processing the images produced. “We’re using our expertise in artificial intelligence system design to improve specific measurements from highly complex data,” explains Demian Wassermann, who is a member of the PARIETAL team (Univ. Paris-Saclay, CEA, Inria) at NeuroSpin. He uses the following analogy to explain his work. “Can you work out the shape of a drum from the sound it makes? In the same way, we can work out the structure of brain tissue from the magnetic echo generated by its activity.” Known as the ‘inverse problem’, this approach consists of determining the causes of a phenomenon from observing its effects. It starts with a modelling stage describing experimentally observable effects, followed by adjustment to this model’s parameters as best as possible based on real measurements. However, when applied to brain imaging, this methodology has a limitation. Due to the current nature of MRI, the smallest observable volume corresponds to a cube of about 1.5 mm³. Each of these “voxels” (which are equivalent to the pixels making up a digital image) contains several thousand cells. Direct observation of the activity of each of them is therefore impossible. Statistical approximation has to therefore be used, to the detriment of the accuracy of the information obtained.
An alternative to this statistical approach is biophysical modelling, based on the spatial characteristics of the elements present in each tissue. However, brain tissue is composed of elements of very different shapes. The somas (cell bodies of neurons) are similar to spheres, while the axons and dendrites which connect them are like long cylinders with a very small diameter. In addition, their distribution in the brain varies significantly, with grey matter containing mostly somas and dendrites, and white matter mostly axons. The complexity of brain structures requires a rethinking of how to use MRI data. “The techniques available for processing this data were not suitable due to their very high dimensionality,” concludes Demian Wassermann. Thanks to techniques such as artificial neural networks and machine learning, it is now easier to model how anatomy and cognitive functioning are linked.
Publications:
- Quettier L. et al, Commissioning completion of the Iseult Whole Body 11.7 T MRI System. IEEE Transactions on Applied Superconductivity, 2020, 30 (4).
- Amadon A., Cloos M. Method and apparatus for compensating for B1 inhomogeneity in magnetic resonance imaging by nonselective three-dimensional tailored RF pulses. Patent WO2011128847 (2011).
- Houenou J., Boumezbeur F. et al. Accumulation of Lithium in the Hippocampus of Patients With Bipolar Disorder: A Lithium-7 Magnetic Resonance Imaging Study at 7 Tesla. Biological Psychiatry, 2020, 88 (5).
- Houenou J. et al. Disruption of Conscious Access in Psychosis Is Associated with Altered Structural Brain Connectivity. Journal of Neuroscience, 2021, 41 (3).
- Jallais M., Wassermann D. Single Encoding Diffusion MRI: A Probe to Brain Anisotropy. In: Anisotropy Across Fields and Scales. (2021).
The limits of neurodevelopment
Technological advances in the field of cognitive science should not lead to mental health being viewed solely from this perspective. This warning has been issued by Bruno Falissard, a psychiatrist and director of the Centre for Research in Epidemiology and Public Health (CESP – Univ. Paris-Saclay, UVSQ, Inserm). “The ‘États Généraux’ (World Conference) on mental health and psychiatry was held in France at the end of September 2021, and the word psychiatry was barely mentioned,” he protests.
As Bruno Falissard points out, “The role of psychiatry is to deal with people who are suffering with their inner selves. The cognitive science paradigm views the brain as a system which processes data. While this works from a scientific point of view, there’s the risk that patients may be steered away from effective treatment.” In the case of autism and hyperactivity, there is one aspect which concerns him in particular. This is the rise in a neurodevelopmental approach. “There’s a growing tendency to consider certain conditions as solely a developmental disorder,” he points out. “Policy-making is very receptive to this line of argument.”
Deviant or different?
To illustrate his point, Bruno Falissard makes a comparison with the changing perception of homosexuality. “After World War II and up until quite recently, homosexuality was considered a psychiatric illness and an example of deviant behaviour.” The definition of a “neurodevelopmental disorder” implies an abnormal development of the central nervous system which results in deviant mental functioning. This idea of “deviance” can be understood from a statistical point of view. It is possible to define a standard of homogeneous mental functioning which corresponds to that of a majority of people, and also, as a consequence, pinpoint those minorities who deviate from it. In the case of autism or hyperactivity, the relevance of this approach can be called into question.
Definitions of these disorders have evolved considerably and now include the idea of a “spectrum” which covers particular mental functions which are often difficult to characterise. Reducing these functions to developmental disorders promotes a simplistic view in that people with different behaviours are solely defined by the abnormal functioning of their brain. Apart from the risk of settling for solutions just involving drugs, this neurodevelopmental approach also denies the fact that today some people claim their situation to be an identity and not an illness. “It’s not a question of denying the reality of severe autism and the confusion resulting from it. In these cases, the cognitive approach is relevant and allows families to feel less guilty,” Bruno Falissard points out. “But covering complex situations with a veneer of rationality carries the risk of treating them poorly. Considering autism as a spectrum is incompatible with the neurodevelopmental approach.”
While this plea has received positive feedback from the psychiatric community, it also echoes the wishes of a growing number of autistic people who hope not to be cured of their autism, but instead to have the difficulties arising from it properly addressed.
Publication :
- Falissard B. Did we take the right train in promoting the concept of “Neurodevelopmental disorders”? European Child Adolescent Psychiatry, 30 (2021).